Umbilical cord blood can be used to treat for diseases such as:
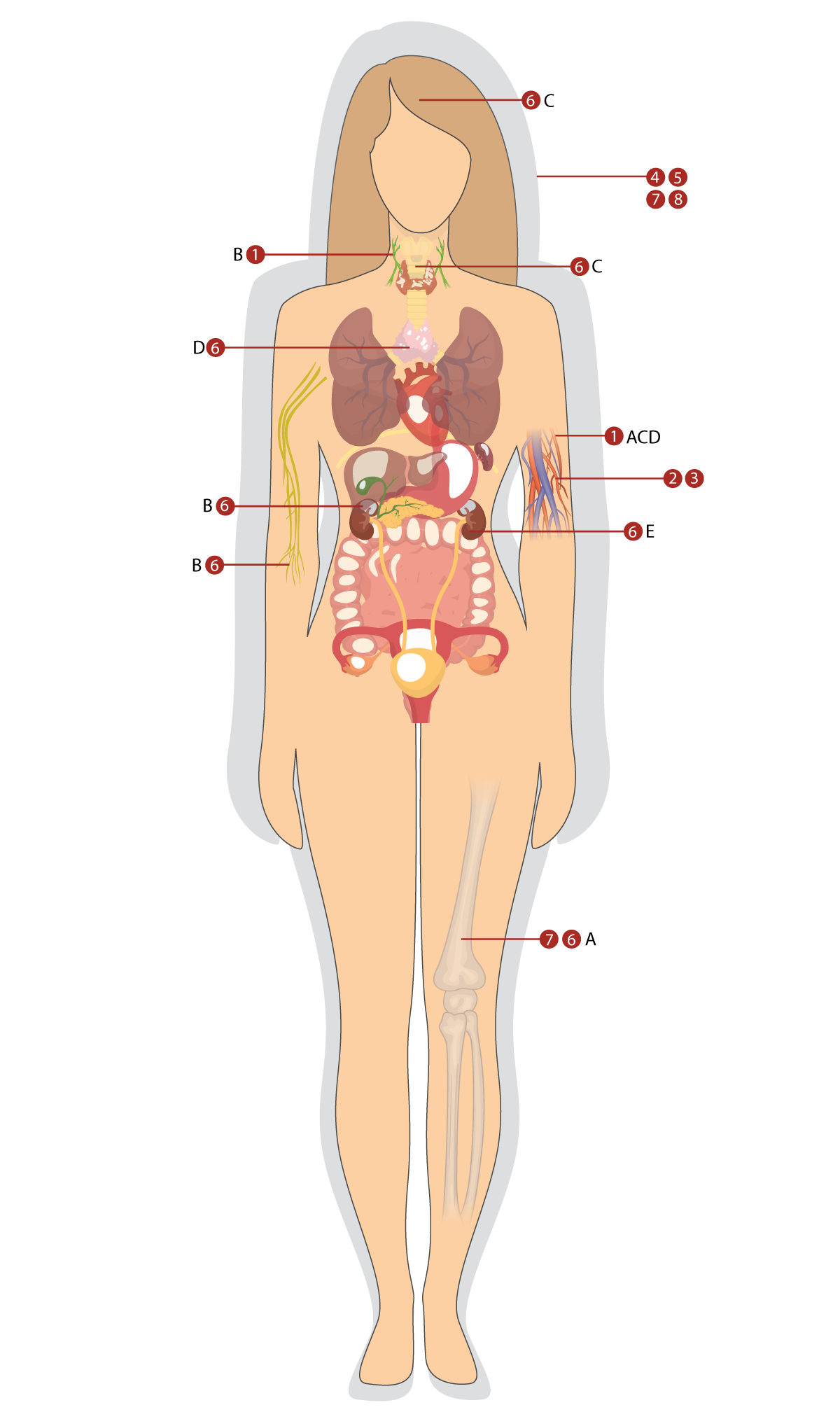
1. Malignant diseases of the blood
-
- Leukaemia
- Acute lymphoblastic leukaemia
- Acute myeloblastic leukaemia
- Lymphomas
- Hodgkin’s lymphoma
- Selected Non-Hodgkin’s lymphomas such as Burkitt’s lymphoma and follicular lymphoma
- Myelomas
- Multiple myeloma
- Myelodysplastic syndromes
- Leukaemia
2. Acquired blood diseases (non-malignant)
- Aplastic anaemia
3. Congenital blood diseases (non-malignant)
- Thalassaemia
- Sickle cell disease
- Fanconi anaemia
- Blackfan-Diamond anaemia
4. Acquired immune disorders
- Multiple sclerosis
- Systemic lupus erythematosus
5. Congenital immune disorders
- Lazy-leukocyte syndrome
- Wiskott-Aldrich syndrome
6. Oncological diseases – malignant solid tumours
- Ewing’s sarcoma
- Neuroblastoma
- Rhabdomyosarcoma
- Thymoma
- Wilms’ tumour (nephroblastoma)
7. Metabolic disorders
- Osteopetrosis
- Tay-Sachs disease
- Gaucher’s disease
- X-linked adrenoleukodystrophy
8. Irradiation disease
Almost 100 serious diseases that umbilical cord blood can be used for:
Sources: https://parentsguidecordblood.org/en/diseases#standard, https://pubmed.ncbi.nlm.nih.gov/26256941/, https://pubmed.ncbi.nlm.nih.gov/22002489/, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5771710/.
 Umbilical cord blood is currently used in the treatment of certain haematological and oncological diseases, such as leukaemias, lymphomas, organ cancers, immune disorders or metabolism disorders. In most of these diseases, hematopoiesis in the bone marrow fails. In bone marrow regeneration using haematopoietic stem cells, we speak of the so-called haematopoietic stem cell transplantation. Umbilical cord blood has already been used in more than 40,000 transplants worldwide.
Umbilical cord blood is currently used in the treatment of certain haematological and oncological diseases, such as leukaemias, lymphomas, organ cancers, immune disorders or metabolism disorders. In most of these diseases, hematopoiesis in the bone marrow fails. In bone marrow regeneration using haematopoietic stem cells, we speak of the so-called haematopoietic stem cell transplantation. Umbilical cord blood has already been used in more than 40,000 transplants worldwide.
Umbilical cord blood has huge potential in regenerative medicine, which deals with the regeneration of damaged tissues and organs.
Nearly 1 in 3 people may benefit over their lifetime from regenerative medicine, including therapies for neurological, cardiovascular, autoimmune and orthopaedic diseases.
Regenerative medicine therapies may be the best hope for patients with a lifetime of disability and impairment. Diseases such as stroke, spinal cord injury and myocardial infarction might be treated with greater efficacy using umbilical cord blood therapy – based approaches rather than current treatment options.
Who can benefit from umbilical cord blood treatment?
Treatment with her/ his own umbilical cord blood (autologous)
Transplantation of one’s own haematopoietic stem cells means that doctors use umbilical cord blood to treat a baby, from whom it has been taken at birth, at any time during its lifetime. Thus, the patient “donates their own cells“. The great advantage is that the body and umbilical cord blood do not fight against each other, and therefore there are no complications after transplantation, which can happen when using cells from another person.
Own umbilical cord blood can be used in treatment in cases where own bone marrow or peripheral blood is used standardly. The need for treatment with own haematopoietic stem cells, as well as the specification of their source, is determined by the attending physician in cooperation with the transplant commission.
With age, there is an increasing frequency of the number of diseases that can be treated and globally more blood-forming stem cells are transported using the patient’s own umbilical cord, peripheral blood or bone marrow (60%) than from donor cells (40%).
Own cord blood is also being used in clinical trials for the treatment of cerebral palsy, autism, traumatic brain injury, spinal cord injury, acute burns and more.
The first results showed that when adequately dosed, cord blood may improve motor function in young children with spastic cerebral palsy.
Storing your child´s cord blood makes them eligible at any time for an autologous treatment.
Although own umbilical cord blood has many benefits, it is sometimes necessary to use umbilical cord blood from a sibling or foreign donor for treatment. In particular, these are cases where the disease is genetically determined and the umbilical cord blood itself would therefore not be an appropriate solution.
Using stem cells from cord blood for a sibling (allogeneic)
Umbilical cord blood can also be used to treat a sick sibling. When using cells from a donor, one of the important indicators of whether it will be possible to transplant umbilical cord blood, is the match of HLA markers. The most preferred donor is a matching sibling.
Compared to the administration of umbilical cord blood from a completely foreign donor, sibling transplants have better results and a lower risk of serious complications after transplantation. The probability that sibling´s HLA markers are matched 100%, is 25%.
If the older sibling is ill and the mother is pregnant at the time, your doctor may recommend collecting cord blood for the needs of the ill sibling. In this case, the parents do not pay for the collection, processing or storage of umbilical cord blood. More about the free collection for an ill sibling.
Treatment with cord blood from a donor (allogeneic)
A donor of cord blood can be an unrelated person. Finding a matching donor is the key to a successful allogeneic transplant. Matching cord blood can be searched in the register of donors of umbilical cord blood. A public registry, the Slovak Placental Stem Cell Registry (Slovenský register placentárnych krvotvorných buniek), as a part of Cord Blood Center Group, is linked to an international database of public registries.
Umbilical cord blood from public registries is used especially for treating leukaemia in children and adults or genetic disorders of blood formation and metabolism in children.
Allogeneic (donated) cord blood has recently became been used in clinical trials for medicine regenerative applications. After initial promising results in the treatment of children with cerebral palsy, to extend this therapy, the possibility of using allogeneic cord blood in adults with ischaemic stroke was considered.
Very often there are misunderstandings about who can use cord blood in treatment. The short answer is it very much depends on the disease being treated. And, finally, it is the doctor’s decision.


N. S. Majhail et al., Biol. Blood Marrow Transplant. 21, 1863–1869 (2015).